Saxenda (liraglutide (rDNA origin)) is a glucagon-like peptide-1 (GLP-1) receptor agonist indicated as an adjunct to a reduced-calorie diet and increased physical activity for the treatment of obesity and chronic weight management.
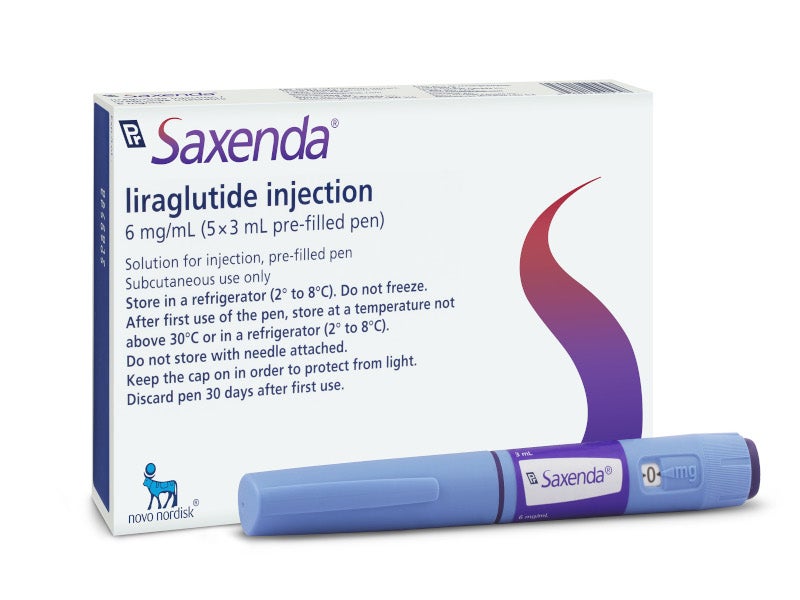
Discovered and developed by Denmark-based pharmaceutical company Novo Nordisk, Saxenda is available as a solution in pre-filled, multi-dose pens that delivers doses of 0.6mg, 1.2mg, 1.8mg, 2.4mg or 3mg for subcutaneous injection.
Regulatory approvals for Saxenda
Novo Nordisk received favourable votes of 14-1 for the approval of Saxenda for weight management from the US Food and Drug Administration’s (FDA) Endocrinologic and Metabolic Drugs Advisory Committee panel in September 2014.
In December 2014, the FDA granted approval for Saxenda for the treatment of chronic weight management, combined with a reduced-calorie diet and physical activity.
The drug is designed for adults with obesity (body mass index or BMI>30) or overweight (BMI>27) and affected with an obesity-related condition such as type 2 diabetes, cardiovascular disease, hypertension or high cholesterol.
Health Canada approved Saxenda for chronic weight management in February 2015. The European Commission authorised the drug for marketing throughout the European Union (EU) to help manage weight in adults in March 2015.
The updated Saxenda injectable 3mg label was approved by the FDA in April 2017, based on findings from the SCALE™ Obesity and Pre-diabetes three-year trial, ensuring long-term safety and efficacy.
A supplemental indication for the drug received approval from the FDA for chronic weight management in obese patients aged 12 years and older in April 2020.
The European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) recommended the use of the drug for treating obesity in adolescents aged 12-17 years in March 2021.
The Scottish Medicines Consortium (SMC) assessed Saxenda and advised NHS Boards and Area Drug and Therapeutics Committees (ADTCs) on its use in NHSScotland in April 2022, resulting in its acceptance for restricted use.
Obesity and its prevalence
Obesity is a weight-related disorder that affects more than a third of adults in the US. The condition can be measured using BMI, the measurement of body fat based on the person’s height and weight.
Obesity can lead to several health issues, including heart disease, type 2 diabetes, certain cancers and a reduced life expectancy.
An estimated 80 million adults in the US suffer from obesity.
Saxenda’s mechanism of action
Saxenda contains an active component called liraglutide, which is a glucagon-like peptide-1 (GLP-1) analogue. The drug, which can be administered intravenously, reaches activated neurons in brain regions and regulates appetite and calorie intake.
Clinical trials on Saxenda
The FDA’s approval of Saxenda was based on results from three Phase III clinical trials SCALE (Satiety and Clinical Adiposity−Liraglutide Evidence in Nondiabetic and Diabetic people) studies, which were conducted for 56 weeks to evaluate the drug’s safety and efficacy.
More than 5,000 participants were enrolled in the three SCALE clinical trials, each of whom was obese or overweight and with or without other weight-related conditions.
The first SCALE clinical trial was a randomised, double-blind, placebo-controlled study. It enrolled 3,731 patients with obesity. The second study enrolled 635 patients with type 2 diabetes, who were either overweight or obese while the third study enrolled 422 patients with obesity.
Patients were given 3mg of Saxenda daily or a placebo for 56 weeks and received counselling about lifestyle changes they needed to adopt related to a low-calorie diet and regular physical exercise.
The primary efficacy parameters of the first and second SCALE clinical studies included the mean percentage change in body weight and the percentages of patients achieving greater than or equal to 5% and 10% weight loss from baseline to week 56.
The third study’s primary efficacy parameters included the percentage change in body weight from randomisation, the percentage of patients not gaining more than 0.5% body weight from randomisation and the percentage of patients achieving greater than or equal to 5% weight loss from randomisation to week 56.
Results from the studies demonstrated that patients treated with Saxenda experienced a statistically significant weight reduction compared with placebo after 56 weeks. Patients treated with Saxenda achieved at least 5% and 10% weight loss compared to placebo.
The most serious side effects reported during the trials in patients treated with Saxenda included pancreatitis, gallbladder disease, renal impairment and suicidal thoughts.